Are you passionate about providing
the best possible care for your residents?


When you’re running a care home, one of the biggest challenges you face is finding the right staff. Then you have to make sure that they deliver care in the way you want them to.
The training you provide is a huge part of that – and that’s where clinicalskills.net can help.
With our highly praised content and e-learning materials, we can help you to stretch your training budget further, support your staff and keep track of training progress. Not to mention being prepared for your next CQC inspection!
Easily monitor staff progress and track their training—stay on top of who has done what and when so you can show the CQC.
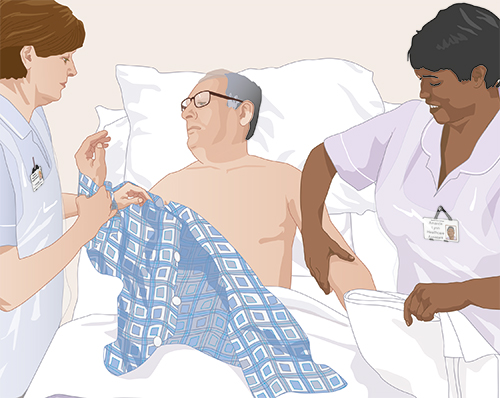
- Fully illustrated step-by-step skills guidelines that are quick and easy to understand
- Content ranges from the Care Certificate through to nursing skills and manual handling, complete with online assessments
- All regularly updated and peer reviewed so you have access to all the latest guidance
- Your staff can access our mobile-friendly website 24/7, and train at a time that’s convenient for them
- CPD and revalidation tools to help your registered nurses and other healthcare staff
- Flexible assessments you can tailor to your local needs
- Download certificates for assessments taken by your staff.
The best way to properly understand how clinicalskills.net can help your care home is to schedule a free demo. This will be online, using Teams or Zoom, and takes around 30 minutes. To get the full picture and understand whether or not clinicalskills.net is right for your care home, click the button above to arrange a demo.
Highly recommended
Working in a nursing home, we were looking for training with higher standards to support our registered nurses. clinicalskills.net has delivered a wider perspective on most topics, providing us with deeper insights and updated information. I highly recommend it.
Fantastic customer service
clinicalskills.net is a fantastic training resource. Staff feedback has been excellent. As training manager, I find it exceptionally easy to monitor staff progress. The customer service is fantastic too – always someone on hand to help me. Well done Clinical Skills.
